#Semaglutide
#Semaglutide
[ follow ]
#glp-1 #weight-loss #wegovy #tirzepatide #novo-nordisk #glp-1-drugs #obesity #fda-approval #clinical-trials #ozempic
from24/7 Wall St.
1 week agoEli Lilly Is Dominating the GLP-1 Wars as Novo Nordisk Sales Tank
Novo Nordisk initially dominated the space with its semaglutide-based drugs, Ozempic for diabetes and Wegovy for obesity, securing a strong foothold in both markets. However, Eli Lilly has since pulled ahead with tirzepatide - marketed as Mounjaro for diabetes and Zepbound for weight loss. The drug's dual GLP-1/GIP receptor mechanism delivers superior weight loss - around 20% in trials compared to semaglutide's 14% - propelling Lilly into the market leadership position.
Medicine
fromFast Company
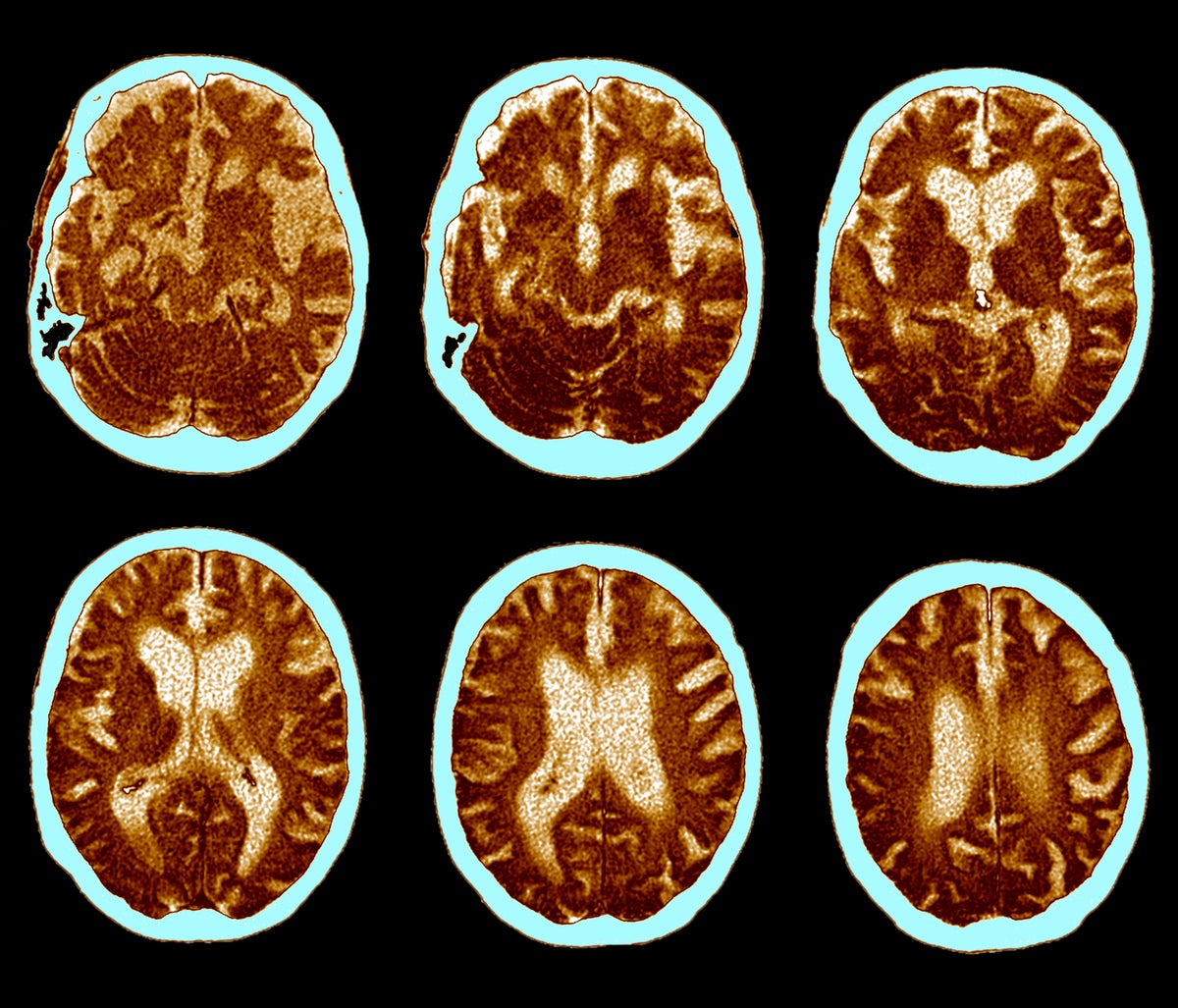
2 months agoNovo Nordisk stock slides as its Alzheimer's drug trials fail
Novo Nordisk's closely-watched Alzheimer's trials of an older oral version of its semaglutide drug failed to help slow the progression of the brain-wasting disease, the firm said on Monday, a blow to the obesity drug giant that sent its shares sliding. The trials, which Novo had previously called a "lottery ticket" to underline its highly uncertain outcome, were testing whether the medicine could slow cognitive decline in patients.
Health
fromNews Center
3 months agoObesity Drugs Regulate Neural Systems to Curb Appetite - News Center
The study, led by Lisa Beutler, MD, PhD, assistant professor of Medicine in the Division of Endocrinology, Metabolism and Molecular Medicine, improves the understanding of the molecular mechanisms influenced by these drugs and could help refine the development of future targeted therapies for treating diabetes and obesity. Incretin receptor agonists are a class of drugs that mimic the effects of incretin hormones - glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP) - to stimulate insulin secretion and regulate blood sugar levels.
Medicine
fromPsychology Today
5 months agoBody Image in the Ozempic Era
Before I explain, I want to clarify that I firmly believe in body autonomy. If someone chooses to take a weight loss medication, they should be able to do so without judgment. I hope all potential users are fully informed about the risks and benefits of these medications and are followed responsibly by medical providers. Ideally, they would also be screened for a current or past eating disorder or any other condition that might contraindicate the use of GLP-1s and GIPs.
Medicine
Right-wing politics
fromThe American Conservative
7 months agoThe FTC Has the Chance to Rein in Big Pharma
Big Pharma's actions regarding necessary medicines, particularly semaglutide, require careful regulation.
Reliance on two manufacturers for crucial diabetes and obesity drugs poses significant risks to patients.
[ Load more ]